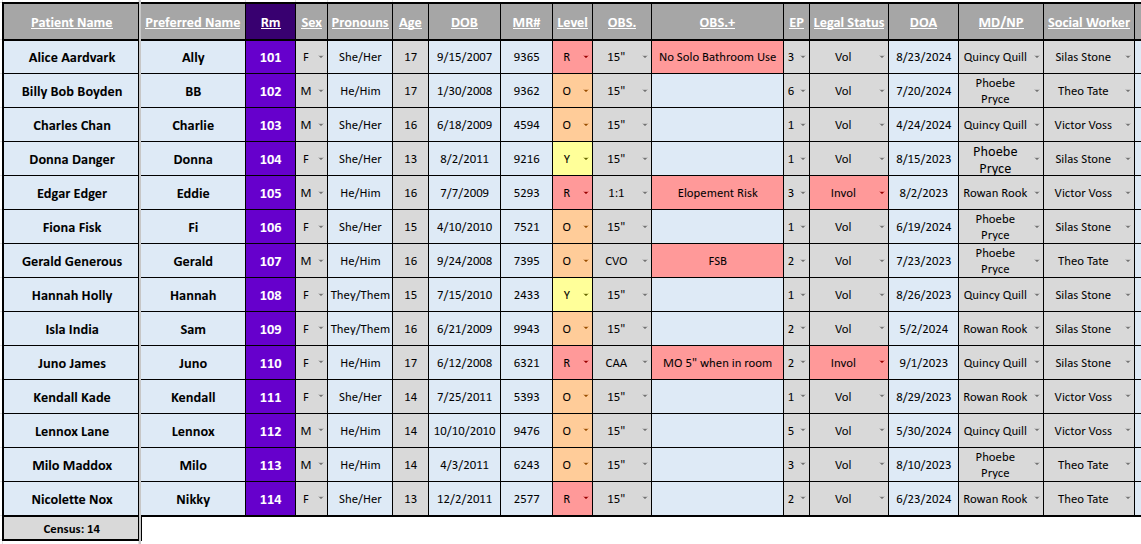
Inpatient Mental Health Unit Smartboard
One year (iterative, continuous improvement)
Tools
Project Goals:
To develop a system that provides the entire care team for a patient at an inpatient psychiatric hospital with timely and accurate information. This system aggregated over several dozen disparate and dynamic pieces of information about the patient into a consolidated data management system used by both administrative and clinical staff. Resulting in more consistent patient care producing measurably improved patient outcomes.
My Role in the Project:
As the project owner I consulted with clinical and administrative staff on existing and previous systems, consolidated historical information into a project plan, sought and obtained management buy-in, and executed the project.
From that background information I developed from scratch a data management system using tools already familiar to the staff to track, manage, display and update critical patient information in the most useful format to the care teams assigned. Taking a page from agile development methodologies I met on a regular basis with the people using the tool to get feedback, develop improvements, and implement changes in a timely manner.
Post implementation, and due to enthusiasm with the tool I was asked by facility leadership to start a training program to deploy the tool across the institution.
Project Challenges:
Creating a data management system that could store and convey the amount of complex information required meant learning and implementing complex functionality in tools the staff was accustomed to. This involved making use of advanced features of MS Excel and underlying database functionality to manage and programmatically update data across the interface.
The lack of easily consumable data export facilities from EMR systems required the construction of staff run procedures for data collection, integration, and sanitation.
The constant variability of clinical interactions required building a system that was both stable, and easy to access, as well as easy to customize and change to meet that variability. Basing the system on generic tools allowed for easy manipulation of the tool requiring it be built in a way that was easy to fix and difficult to introduce errors.
Staff communication across multiple shifts made getting feedback challenging at times, this, along with normal change aversion often made it difficult to find the (functionality? Form factor? Presenting the information in ways all staff could understand/access). Getting buy-in from staff required a road show like roll out to get people on board with changes intended to make their jobs easier.
Lack of overall technical training within clinical settings required skill updates and training to allow staff to fully engage with the new tooling.
Results and Outcomes:
The system as implemented, significantly decreased informational errors across clinical shifts resulting in improved patient comfort and clinical outcomes.
Greater access to clinical information reduced treatment times and turn around times for problem escalation and resolution, especially for time sensitive concerns.
Dramatically improved data management reduced interdepartmental friction, smoothing both admissions, clinical administration and overall staff frustration.